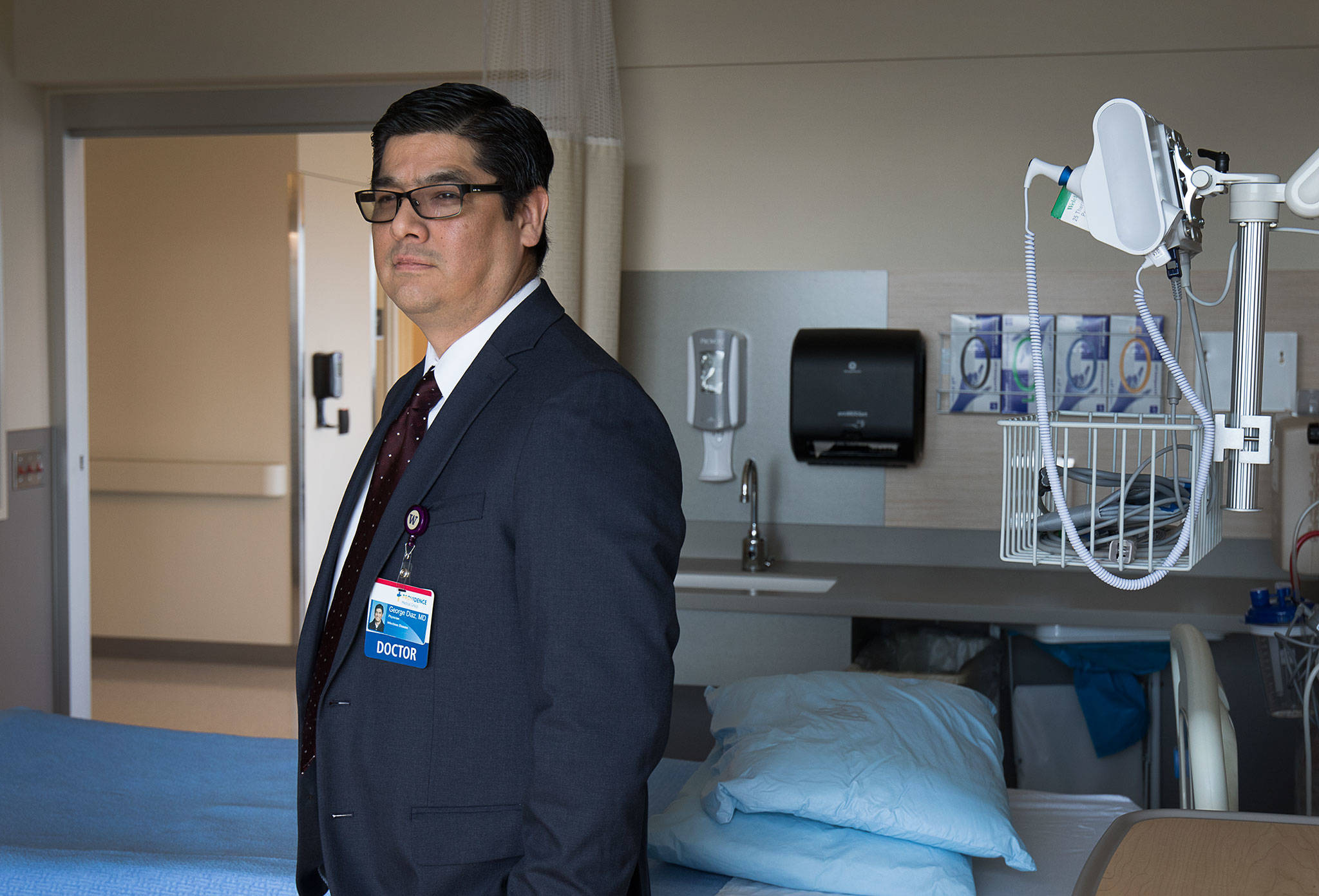
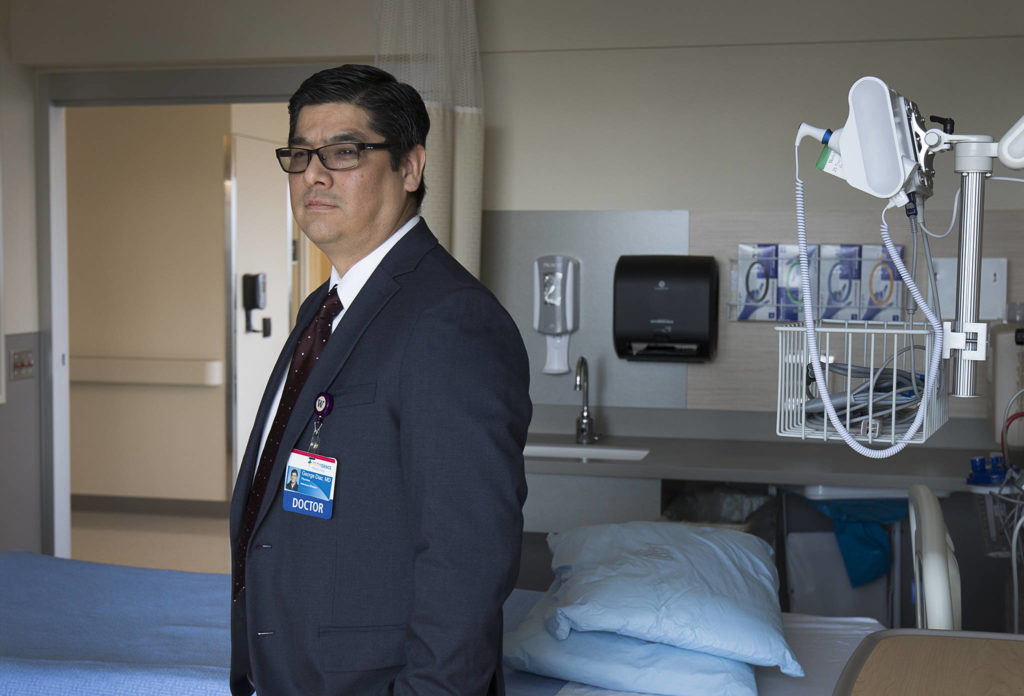
EVERETT — Two weeks ago, Dr. George Diaz worried where the supplies would come from to fight an expected surge of COVID-19 patients.
Providence Regional Medical Center Everett, the county’s largest hospital and intensive care unit, needed more beds, more ventilators, more staff, and maybe most of all, more protective equipment.
The hospital had burned through more gowns, gloves, and masks in a month than the entire 51-hospital system uses in a typical year.
“The concern initially was are we going to have enough … to keep going?’’ said Diaz, 48, an infectious disease specialist overseeing the hospital’s response to the virus.
On Wednesday, a more confident Diaz sat in his windowless third-floor office at Providence and talked about what had changed.
At one point, he held up a blue hospital-quality surgical mask manufactured by Kaas Tailored of Mukilteo.
“This,” he said, “is a lifesaver.”
Contributions like those from Kaas, one of several local manufacturers who converted their operations to produce badly needed supplies, have played a big role in helping Providence and other facilities to prepare for an expected wave of critically ill patients later this month, when the outbreak is expected to peak in Snohomish County.
“Although the (hospital) system is stressed, it’s not cracking,” said Dr. Chris Spitters, health officer for the Snohomish Health District.
Finding a new source for critical supplies is just one of several measures that administrators at Providence said they’ve taken in recent weeks to ready themselves.
“The things you worry about with this are fairly limited,” Diaz said. “Do you have enough staff? Do you have enough supplies? Do you have enough beds?”
Providence canceled many outpatient services and non-emergency surgeries, in the process freeing up staff and beds, as well as saving protective gear. They also rented and repurposed ventilators to create more intensive care beds, and they discharged patients no longer requiring hospital care to free up space.
But maybe most helpful has been a social distancing policy that seems to be slowing the spread of the virus, Diaz said, noting the number of Snohomish County hospital patients with COVID has flattened over the past week or so.
“It had been rising,” he said. “Hopefully that indicates we’re getting close to the peak here and we’re just waiting for a drop to happen where we actually see the patient census go down. We’re preparing in case those numbers go up, but that hasn’t really been seen yet over the last week or so.”
The latest modeling from the University of Washington suggests the peak, in terms of infections, could be reached in Snohomish County about April 11. A rise in hospital admissions is expected seven to 10 days later. How big a rise is still unknown.
On Wednesday, Providence was treating about 75 patients who had either tested positive for the virus or were awaiting results, Diaz said, and while not expected, the hospital “could easily handle double that.”
“We’ve got enough capacity to manage what we’d expect during a surge,’’ Diaz said.
It’s a similar story at EvergreenHealth Monroe, another of the county’s four acute-care hospitals, along with Swedish Edmonds and Cascade Valley Hospital in Arlington.
“Overall, we definitely feel better,” said Dr. Midori Larrabee, the hospital’s chief medical and quality officer. “We’re doing a really good job planning and anticipating and coordinating. … It’s just waiting to see what this surge looks like and making sure we’re ready for it. “
Still, Larrabee is wary.
“We don’t know what’s coming,” she said.
Currently, the 31-bed hospital is about half-full, and the majority are non-COVID-19 patients, she said. A shuttered maternity ward and an ambulatory ward could be converted if more space is needed. The hospital has six ventilators.
For now, the hospital “has a good handle” on other supplies, she said, including protective equipment.
“Like everybody in the region, we don’t know when or if we’re able to get more,” she said. “There’s a lot of fear out there.”
Of eight Monroe employees tested for the virus, one returned a positive result.
Facing danger
The shortage of protective equipment and the continual relaxation of best-practice standards have angered some frontline workers.
On March 20, nine Snohomish County health care workers had tested positive for the virus. By Friday, that number had swelled to 76.
At Providence, some nurses work a 12-hour shift with one protective mask, said Katherine Piana, a registered nurse in the emergency room.
“We were the first hospital in the U.S. to have a confirmed case — six weeks later, we’re still suffering from a serious lack of supplies,” said Piana, who joined other nurses from across the state and Sen. Patty Murray at a Friday press conference, calling on hospital administrators to be transparent about personal protective equipment supplies.
Sometimes the gear nurses get from administrators doesn’t fit and the hospital has threatened to fire staff that bring in their own masks, Piana said.
She also said administrators don’t always tell staff if they’ve been exposed to the virus.
Employees who are notified and put in quarantine then have to use their paid time off and sick leave, she said.
The group called for hazard pay and paid leave for the virus.
Meanwhile, at least two Providence Everett nurses contacted a Seattle law firm seeking to get the word out about what they considered unsafe working conditions.
In a statement released Wednesday, the nurses, who said they feared losing their jobs if they publicly criticized Providence, complained about the reuse of protective equipment, something they said would have been forbidden a few weeks before. They also detailed changing protocols for dealing with COVID-19 patients and a lack of testing that put them more at risk of contracting the virus.
The hospital encouraged healthcare workers to create advance directives to ensure their end-of-life wishes were met, they said, indicating Providence “is fully aware of danger they face.”
“The last couple of weeks have been pretty tough in terms of staff verbalizing our concerns about (protective equipment) and really pushing and encouraging them to do the right thing,’’ said Matthew Skews, 52, of Lake Stevens, who works in interventional surgical services at Providence.
Prior to that, Skews said, some staff were being told they had no reason to wear a mask, or weren’t working with patients that warranted a mask, or might scare patients by wearing one. Even people who brought their own masks were discouraged from wearing them or even had them taken away, he said.
“We need to know we’re not bringing this stuff home to our family,” Skews said. “If we bring this home to our families, then what? Or if we get sick ourselves, then what?”
Skews said several Providence nurses with mild symptoms have tested positive for the virus. Others are awaiting results.
‘Stressed to the max’
Given the nationwide shortage of protective equipment, Diaz said the hospital made it clear to staff they were trying to preserve as much as possible. Providence always followed the U.S. Centers for Disease Control and Prevention guidelines on the proper use and reuse of supplies, hospital officials say.
“We want to make sure they were using it absolutely appropriately every single time,’’ Diaz said. “If someone starts using our (personal protective equipment) in a way that’s confusing, that does send a mixed message to the staff. This stuff is like gold. It protects people’s lives. We have to value it and that’s the message we’re giving our staff.”
As supplies become more available, more protection is being provided. On March 27, Providence adopted universal masking, a voluntary option that allows caregivers in clinical settings, or those who handle food or medical supplies, to wear a medical-grade mask they get from their unit leader at the beginning of each shift. The policy doesn’t limit the number of masks available to caregivers caring for patients in isolation. Masks are still being reprocessed to ensure a large enough supply.
Hospital officials say they’ve regularly encouraged caregivers to complete advance directives for almost five years.
“I can tell you there’s nothing more important for our hospital leadership than keeping our staff safe,” Diaz said. “That’s been the number one priority this whole time.”
Some hospitals in the state continue to keep masks under lock and key and are telling employees they can only be worn in certain situations, said Ruth Schubert, communications director with the Washington State Nurses Association, which represents 19,000 nurses statewide, including 15 with the Snohomish Health District.
Some are also warning employees not to talk to the media.
“We’re pretty horrified that nurses aren’t able to speak out,” Schubert said. “We feel pretty strongly that they’ve got to unmuzzle frontline healthcare workers so that people know what they’re facing.”
Robin Strine, a lab employee at Swedish Edmonds, got tested and sent home last week after she experienced a sore throat, headache and an upset stomach, she said. She was waiting for her results.
“My greatest fear is that I end up in the hospital in the ICU intubated or have my family exposed,” she said. “Unfortunately, the way things are going I feel it’s probably not if but when we’re all going to be exposed.”
Strine, of Brier, said she believed Swedish was doing all it could to provide protective equipment for its workers.
“It’s a worldwide shortage now,” she said. “It’s just making sure it’s disbursed equitably and the people needing it are getting it. That’s the important thing — that we’re all taken care of.”
Staff at Swedish Edmonds, she said, are “stressed to the max.”
“Everybody is exhausted and concerned, and that makes it hard on everybody,” she said.
For Diaz, 16-hour days are the new normal. Some days he sees 20 to 25 patients. Other days he meets with hospital administrators, reviews cases and manages two clinical trials of COVID-19-related drugs.
“There’s endless amounts of work,” said Diaz, who treated the nation’s first COVID-19 patient in January.
He misses playing soccer two or three nights a week with coworkers and attending his kids’ soccer practices.
“I go home, my wife makes me dinner, I relax a little bit and then go to bed,” Diaz said.
Even then, sometimes sleep doesn’t come.
“The biggest thing that keeps me up is keeping us on top of stuff that we need to be able to share with the world,” he said, “because there’s so much information being generated by not only our hospital, but our health system. This stuff needs to be published … so that others can benefit from our experience.”
Herald writer Joey Thompson contributed to this story.
Phillip O’Connor: 425-339-3480; poconnor@heraldnet.com. Twitter: @phillipoconnor3
Talk to us
> Give us your news tips.
> Send us a letter to the editor.
> More Herald contact information.